MERGE X TRANSMIT Data Brief #3: Healthcare Access Crisis in Lebanon
The data analyzed in this data brief clearly demonstrate that the political and economic crises that have struck Lebanon in the past years poses an immediate risk to population health. A majority of respondents surveyed struggle to access healthcare services and medication. While the marginalized Syrian population remains particularly vulnerable to healthcare exclusion, our analysis shows that a growing share of the Lebanese host population faces similarly precarious conditions. The Lebanese state meanwhile has shown itself unable to respond to this healthcare crisis thus opening the door for further crises such as the recently observed Cholera outbreak.
 Simon Ruhnke, Michele Scala, Fadi Wahbi, Nader Talebi
Simon Ruhnke, Michele Scala, Fadi Wahbi, Nader Talebi
Download the Pdf English version here, Arabic version here.
June 2023
Introduction
Amidst a multitude of crises, Lebanon has seen the emergence of a new group of modern day Robin Hoods. Bank customers, like Sali Hafiz, a 28-year-old Lebanese interior designer have taken matters into their own hands by forcefully retrieving money from Lebanese Banks. But unlike the hero of British folklore, the funds these vigilantes are stealing at (toy-) gunpoint are in fact their own savings, withheld by the banks as part of Lebanon's strict capital control measures introduced in the wake of the country's massive foreign-exchange deficit. What drives these individuals to such desperate measures? A common motivation mentioned by many of these publicly celebrated bank robbers is the need to cover dramatically rising healthcare costs in the wake of Lebanon's economic collapse.
The economic crisis that Lebanon is facing since 2019 has been described as one of the worst in the world in more than a hundred years[1]. The devaluation of the Lebanese Lira of over 90% vis-a-vis the dollar, hyper-inflation (171% annual inflation in 2022) and the economic fallout of the COVID-19 pandemic as well as the war in Ukraine have crushed the economy of the Lebanese Republic. This economic fallout is perpetuated by a void of political leadership and widespread corruption[2]. Since October of 2022, as the political elite cannot come to an agreement, the country finds itself without a president, and with only a caretaker government in place.
The Lebanese healthcare sector has long been criticized for its level of privatization, high cost and exclusivity.[3] The ongoing crisis in the country has further raised these existing access barriers. Skyrocketing cost of healthcare and medication as well an exodus of healthcare staff have rendered vital healthcare unaffordable for many people in Lebanon. One group assumed to be particularly vulnerable to the effects of the crisis are the estimated 1.5 million Syrians who have sought refuge in neighboring Lebanon since the onset of civil war in Syria in 2011[4] and that have since faced considerable political, social and economic marginalization.
This data brief provides evidence on the extent of the medication and healthcare crisis in Lebanon and investigates how both the Lebanese and Syrian population in the country are impacted. It does so using new survey data collected as part of the TRANSMIT research project (s. Box 1) and positioning it within the ongoing discussions over the consequences of the Lebanese crisis.
Data
The Data presented in this brief was collected in a face-to-face survey conducted in Lebanon between October and December 2022 across 43 sampling locations (s. Figure 1). The 2508 observations are evenly stratified between Syrian and Lebanese respondents (henceforth referred to as the sampling strata). The survey is part of a multi-year study that aims at following a representative sample of the Syrian population in Lebanon, as well as the Lebanese host population that resides in the same neighborhoods that was first collected in 2019. The results here are thus not representative for the Lebanese population at large, but rather a selected sample from neighborhoods with a large Syrian representation.[5]
|
Box 1: TRANSMIT – Transnational Perspectives on Migration and Integration TRANSMIT is a migration research project of the DeZIM-Forschungsgemeinschaft and funded by the German Federal Ministry for Family Affairs, Senior Citizens, Women and Youth (BMFSFJ). The project studies the complex interplay of migration dynamics, migrant wellbeing and integration processes by building a transnational data-infrastructure that collects and links quantitative and qualitative data and knowledge on origin-, transit-, and destination countries. In addition to Lebanon, TRANSMIT collects data in Turkey, Morocco, Italy, Nigeria, Senegal, the Gambia, and Germany. |
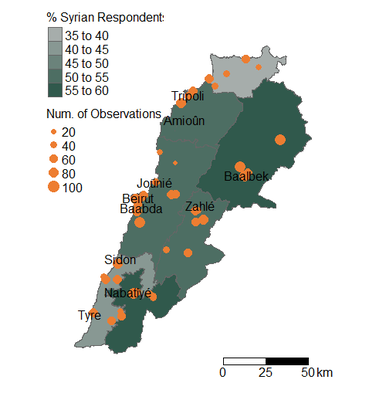
Figure 1: Sample distribution by strata and number of observations
Source: TRANSMIT (2022)
The demographic composition of the sample is displayed in Table 1. The gender balance in both Syrian and Lebanese strata is close to even with a slight female overrepresentation among Lebanese respondents. Syrian respondents meanwhile are on average younger and live in larger households.
|
|
Host |
Syrian |
Overall |
|
Gender |
|
|
|
|
male |
588 (46.9%) |
623 (49.7%) |
1211 (48.3%) |
|
female |
666 (53.1%) |
631 (50.3%) |
1297 (51.7%) |
|
Age Group |
|
|
|
|
15-29 |
369 (29.4%) |
482 (38.4%) |
851 (33.9%) |
|
30-44 |
430 (34.3%) |
557 (44.4%) |
987 (39.4%) |
|
45-59 |
283 (22.6%) |
172 (13.7%) |
455 (18.1%) |
|
60+ |
172 (13.7%) |
43 (3.4%) |
215 (8.6%) |
|
Household Size |
|
|
|
|
Mean (SD) |
3.95 (1.71) |
4.94 (2.22) |
4.45 (2.04) |
|
Median [Min, Max] |
4.00 [1.00, 11.0] |
5.00 [1.00, 13.0] |
4.00 [1.00, 13.0] |
|
Missing |
1 (0.1%) |
1 (0.1%) |
2 (0.1%) |
Table 1: Demographic sample characteristics by strata
Source: TRANSMIT(2022)
Crisis Poses Direct Health Risk
The multi-dimensional crisis in Lebanon poses a direct health risk to the population in the country. As described in our previous data brief, the reliance on imports to cover basic consumption needs and the plummeting value of the Lebanese Pound have resulted in wide-spread food insecurity, further exacerbated by the rising world market prices for wheat and other foodstuffs following the war in Ukraine. In late 2022, insufficient energy supply to maintain water filtration systems and vaccine shortages contributed to the first major outbreak of Cholera in Lebanon in the past 30 years. As of March 2023, the waterborne disease has resulted in 6700 infections and 23 deaths. Due to a lack of sanitation infrastructure, Syrians living in informal settlements in the hard-hit Bekaa valley are particularly vulnerable to the outbreak.
These risk factors come in addition to the increased disease burden following the COVID-19 Pandemic, the management of which was also affected by the crisis conditions in Lebanon. An underfunded public healthcare system and a lack of disease surveillance limited the state’s ability to contain the spread, which ultimately rendered strict lock-down measures necessary.[6]The 50.3% of the population that have received at least one dose of a COVID-19-Vaccine by the end of 2022 also falls far short of the government's goal of 70% vaccine coverage6 leaving nearly half the population at increased risk of severe infection.
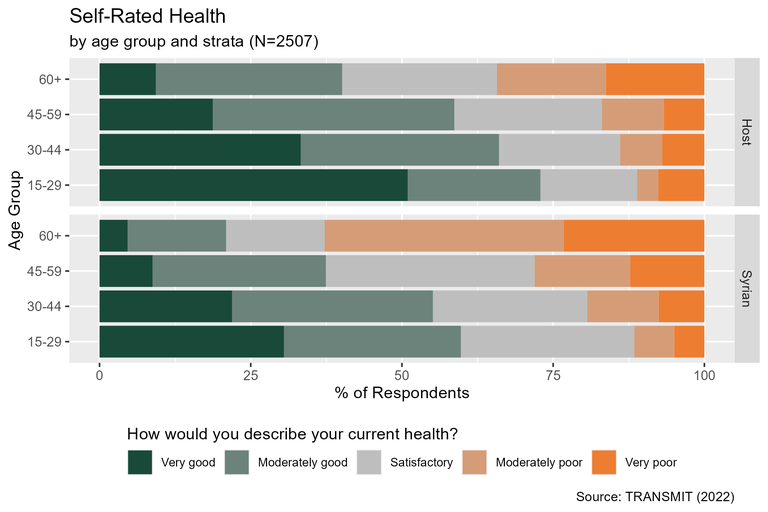
Figure 2 Self-rated health by age group and strata
Evidence for an increased health burden following the Lebanese crises also emerges in our data. During the first TRANSMIT data collection in Lebanon in 2019, 11.9% (Syrian 13.9%, Host: 9.27%) of respondents described their health as moderately or very poor. This rate of poor self-rated health has increased to 17.8% (Syrian: 19.1%, Host: 16.6%) in 2022. Despite being on average younger than their Lebanese counterparts, the health burden appears to be particularly pronounced among Syrian respondents. As Figure 2 illustrates, Syrian respondents in our sample report worse self-rated health across all age groups. The disadvantage is particularly pronounced among individuals aged 60 and above. Over 60% of Syrians in this age group report their health as moderately or very poor.
One aspect of population health that is still too rarely discussed is the topic of mental health. Here too, both Lebanese and Syrian individuals experience numerous risk factors in the wake of the country's crisis. But again, the Syrian population seems to be particularly burdened due to their often-precarious status. According to the PHQ-8 screening tool used in the TRANSMIT surveys, 28.4% of Lebanese, and 45.2% of Syrian respondents display symptoms of an elevated mental health burden.[7] These rates are again substantially higher than in the 2019 wave of the TRANSMIT surveys, where 19.6% of Lebanese and 24.7% of Syrian respondents screened positive. While mental health and psychosocial services are available to refugees through NGOs and international organizations, these are reported to lack sufficient funds to address the growing demand[8] and are not always able to meet the
needs that are expressed by the Syrian refugees themselves and that go beyond immediate clinical care.[9]
Medical Remittances and Aid NOT Enough to Ensure Access to Medication
Lebanon is highly reliant on imports to cover its demand for medical supplies and medication. For years, these imports of essential goods were subsidized by the Lebanese government to ensure they remained accessible to the entire population. In the wake of the devaluation of the Lebanese Lira and the scarcity of foreign currency at the Lebanese Central Bank, this subsidy program was discontinued. In November 2021, the Lebanese government cut back on subsidies for a number of medications, forcing patients to cope with substantial increases in the cost of essential pharmaceutical products such as insulin. In addition to the direct threat these austerity measures pose to patients' health, they also leave healthcare providers struggling with widespread shortages of anesthetics and other medical supplies essential to adequate healthcare provision.
Faced with these shortages, for many households, friends and family abroad have emerged as a critical source of essential medications as visiting expats return with suitcases filled with medications. This access channel is primarily available for the more affluent, well-connected and cosmopolitan elite and leaves the most vulnerable, including the Syrian refugee population, with no option but to seek medication on the largely unaffordable domestic market, through aid organizations or through the clientelist system of political and faith-based organizations which often aim at reinforcing existing dependencies and power structures in Lebanon.[10]
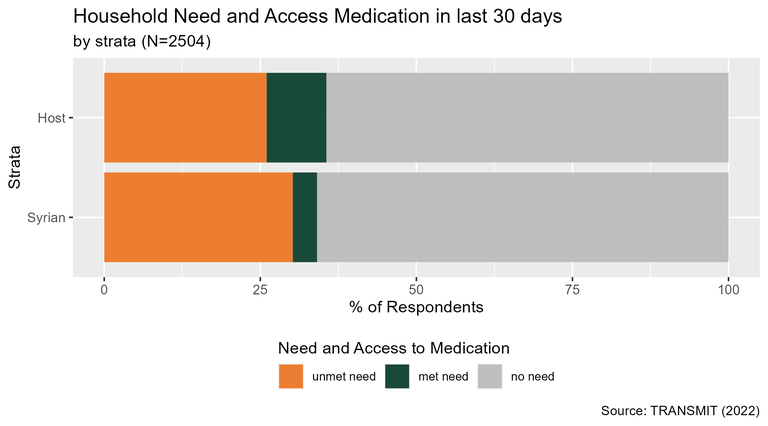
Figure 3 Household need and access to medication in the last 30 days by strata
Our data demonstrates just how widespread unmet healthcare needs are in Lebanon. In our sample, 34,9% of households have at least one member who requires regular medication. Of these households with a medication need, 80,6% (Syrian: 88.3%, Host: 72.9%) reported that they were unable to acquire all medications needed within the last 30 days. Figure 3 illustrates that while the need for medication is similar between Syrian and Lebanese households, Syrians are particularly disadvantaged when it comes to accessing these medications. This is likely a result of both their low economic status, as well as a lack of connection to informal distribution structures (e.g. political parties, religious and philanthropic organizations).
Dwindling Access to Healthcare Services as Healthcare Staff Leaves
The Lebanese healthcare sector is largely privatized. Only 15% of all hospital beds in the country are in public institutions.6 Besides the previously mentioned challenge in reacting to a public health crisis, this level of privatization also threatens to exclude those members of society unable to cover the substantial costs of private care. The Syrian population in Lebanon is particularly vulnerable to this exclusion. Without any formally recognized entitlement to social protection under Lebanese law, most Syrians have to rely on underfunded programs run by NGOs and international organizations to access healthcare[11].
In addition to the wide-spread shortage of medical supplies and the overall increase in costs, the ability of the Lebanese healthcare sector to provide vital care to the population is further hit by the substantial emigration of healthcare staff in reaction to the crises. According to the head of the Lebanese union of medical doctors, more than 3500 doctors left the country between October 2019 and 2022. While official numbers are not available, it is estimated that 40% of medical doctors and 30% of registered nurses left Lebanon by September 2021.6
Our data suggests that the impact of the Lebanese crises on healthcare access was felt particularly hard by the Lebanese population. This is not because the Syrian population enjoyed easier access to care than their Lebanese counterparts, but rather, because Syrian access to care was already extremely challenged prior to the escalation of the economic crisis. During our first wave of data collection in 2019, roughly 80% of Syrian respondents reported that it would be moderately or very difficult for them to see a medical doctor. By 2022, this rate had increased slightly to 83.3%. For the Lebanese population meanwhile, the corresponding rate of perceived difficulty in accessing a medical doctor rose from roughly 50% in 2019 to over 73% in 2022, thus converging towards the poor healthcare access of the Syrian refugee population.
This convergence of the two populations towards a state of poor healthcare access is further evident in the rates of healthcare utilization recorded in our survey in 2022. Roughly two-thirds in both survey strata reported that they had seen a medical doctor about their health in the past year (Syrian: 64.7%, Host: 65.6%). For comparison: The corresponding rate of medical consultations in the previous 12 months is 82.4 % in the EU and 82.7% in Turkey.[12]
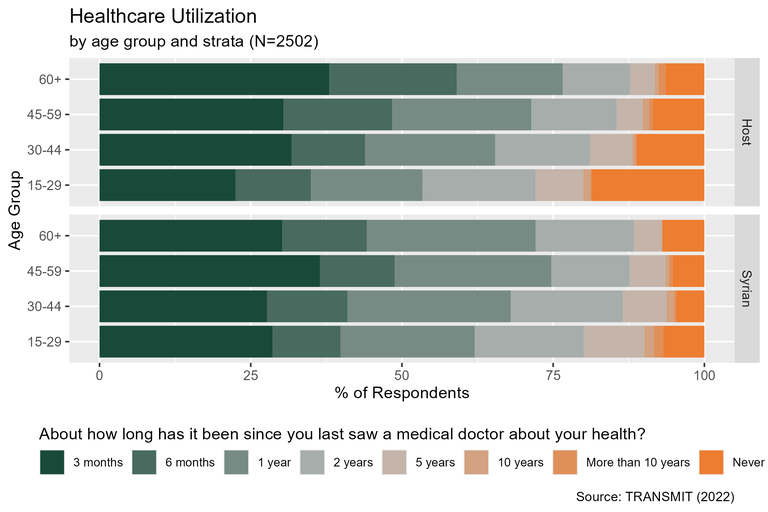
Figure 4 Healthcare Utilization by age group and strata
The differences between Syrian and Lebanese respondents are particularly pronounced for older age groups (Figure 4). While the frequency of healthcare utilization usually increases over age of a population, this pattern does not emerge in the Syrian sample. This pattern is further evidence of the poor healthcare access as it points to a lack of routine care of Syrians (particularly vital for the elderly) and instead, care being provided on a humanitarian basis by aid organizations.
The Breakdown of the Social Protection System Results in Dependence on Clientelist Sectarian Healthcare.
The breakdown of the Lebanese social protection system has further undermined healthcare access in the country. Many observers have criticized the system as elitist and exclusive[13]. Despite its flaws, the social protection framework in Lebanon played a crucial role in alleviating poverty and providing healthcare services prior to the current crisis. According to a study conducted by the International Labor Organization (ILO), as of 2019, approximately two-thirds of Lebanese citizens and half of the non-Lebanese population had access to at least one social protection benefit, including humanitarian aid[14].
In a highly privatized healthcare sector, public social security schemes (the National Social Security Fund (NSSF) in the private sector, and the cooperatives for civil servants, military personnel, and security forces in the public sector) provided access to an otherwise expensive and often unaffordable healthcare system. However, starting in October 2019, the meltdown of Lebanese financial capitalism and the subsequent devaluation of the local currency against the USD gradually led to the de facto collapse of the social protection system and its social security schemes. Consequently, healthcare providers, particularly hospitals, began refusing third-party payments from the publicly mandated social security funds.[15]
The breakdown of the social protection system has far-reaching consequences, leading to profound loss of social status and class downgrading for previously "privileged" populations who were reliant on accessing healthcare services through social security, particularly the "salariat." The rapid and brutal degradation of the social security scheme’s effectiveness helps explaining the diminishing gap in healthcare access between Lebanese and Syrian populations. The continous social downgrading and shrinking disparity in socioeconomic status are evident in the TRANSMIT data. In the 2020 wave of our data collection 59% of Lebanese and 80% of Syrian respondents reported that their household income was insufficient to purchase basic goods and services such as food, electricity or education. These already alarming numbers have since further increased and converged to 81% and 96% for Lebanse and Syrians respectively in the 2022 survey.
In this context, Lebanese residents who are unable to secure private insurance are left with few options. They must either cover the punishingly high expenses out-of-pocket, seek humanitarian support (especially refugee and migrant populations), or rely on political and clientelist networks. As noted by numerous scholars, the so-called "sectarian welfare" historically represents a structural rather than palliative mechanism within the Lebanese social protection framework[16]:
"many hospitals are run by political parties and charities, and offer services under philanthropic pretenses, though it is often on a clientelist basis. In other words, sectarian welfare has established the basis for an actual 'bricks and mortar clientelism'[17], comprised of hospitals and charities founded and operated by political parties, largely financed by public expenditures" (Scala 2022: 22).
However, sectarian welfare primarily addresses the voting population - i.e., Lebanese citizens – that constitutes the power base of traditional sectarian parties. Therefore, in a context characterized by rapid pauperization and class degradation, healthcare access becomes increasingly subject to politicization strategies, or reliant on humanitarian aid and support from non-state actors.
Conclusion
The data analyzed in this data brief clearly demonstrate that the political and economic crises that have struck Lebanon in the past years poses an immediate risk to population health. A majority of respondents surveyed struggle to access healthcare services and medication. While the marginalized Syrian population remains particularly vulnerable to healthcare exclusion, our analysis shows that a growing share of the Lebanese host population faces similarly precarious conditions. The Lebanese state meanwhile has shown itself unable to respond to this healthcare crisis thus opening the door for further crises such as the recently observed Cholera outbreak.
Faced with a collapsed social protection system, large shares of the population in Lebanon become even more dependent on the country clientelist system. Rather than increasing the pressure on the political elite, the dramatic healthcare crisis may actually strengthen the corrupt sectarian structures that many see at as its main cause. In order to mitigate human suffering in the wake of the described healthcare crisis, humanitarian aid to both Lebanese and Syrian populations need to be extended directly while avoiding reinforcing the existing dependencies created by clientelism.
Notes
[1] The World Bank. (2021, June 1). Lebanon Sinking into One of the Most Severe Global Crises Episodes, amidst Deliberate Inaction. https://www.worldbank.org/en/news/press-release/2021/05/01/lebanon-sinking-into-one-of-the-most-severe-global-crises-episodes
[2] World Bank. (2020). The Deliberate Depression (Lebanon Economic Monitor (LEM)). World Bank. http://documents.worldbank.org/curated/en/394741622469174252/pdf/Lebanon-Economic-Monitor-Lebanon-Sinking-to-the-Top-3.pdf
[3] Leenders, R. (2004). Nobody Having too Much to Answer for: Laissez-Faire, Networks, and Postwar Reconstruction in Lebanon. In S. Heydemann (Ed.), Networks of Privilege in the Middle East: The Politics of Economic Reform Revisited (pp. 169–200). Palgrave Macmillan US. https://doi.org/10.1057/9781403982148_6
[4] UNHCR. (2023, May 6). Lebanon Crisis Response Plan—Support to Lebanese in 2022. UNHCR Operational Data Portal (ODP). https://data.unhcr.org/en/documents/details/100499
[5] The sampling frame consists of a list of regions on three levels: the 16 administrative regional units (states), divided into several Primary Sampling Units (PSUs), each again divided into several blocks. On the highest level, all administrative units are selected. From there, multi-stage proportional stratified sampling is applied. From the PSUs within the 16 administrative units those are selected where UNHCR data indicates Syrian presence (including informal settlements, Balanche and Verdeil, 2015). Within the PSUs, the blocks and households are selected randomly. The number of interviews per unit is determined by the size of the overall population.
[6] Hassan, F. F. A., Hamdan, M. B., Ali, F., & Melhem, N. M. (2023). Response to COVID-19 in Lebanon: Update, challenges and lessons learned. Epidemiology & Infection, 151, e23. https://doi.org/10.1017/S0950268823000067
[7] An elevated mental burden is defined here as a sum-score across the 8 Questions of the Population Health Questionnaire (PHQ-8) of greater than 10. The PHQ-8 is merely used as a screening instrument for depression, but as its results are not comparable to rates of clinical diagnosis, we refer to it as a measure of not further specified and/or pathologic mental health burden."
[8] Naal, H., Nabulsi, D., El Arnaout, N., Abdouni, L., Dimassi, H., Harb, R., & Saleh, S. (2021). Prevalence of depression symptoms and associated sociodemographic and clinical correlates among Syrian refugees in Lebanon. BMC Public Health, 21(1), 217. https://doi.org/10.1186/s12889-021-10266-1
[9] Kerbage, H., Marranconi, F., Chamoun, Y., Brunet, A., Richa, S., & Zaman, S. (2020). Mental Health Services for Syrian Refugees in Lebanon: Perceptions and Experiences of Professionals and Refugees. Qualitative Health Research, 30(6), 849–864. https://doi.org/10.1177/1049732319895241
[10] Cammett, M. (2014). Compassionate Communalism: Welfare and Sectarianism in Lebanon. Cornell University Press. https://www.jstor.org/stable/10.7591/j.ctt5hh11g
[11] Singh, N. S., Dingle, A., Sabra, A. H., DeJong, J., Pitt, C., Mumtaz, G. R., Sibai, A. M., & Mounier-Jack, S. (2020). Healthcare financing arrangements and service provision for syrian refugees in Lebanon. In Health Policy and Systems Responses to Forced Migration (pp. 53–76). Springer International Publishing.
[12] Self-reported time elapsed since last visit to a medical professional by sex, age and educational attainment level [HLTH_EHIS_AM1E], European Commission. Statistical Office of the European Union. (2018). European Health Interview Survey (EHIS wave 3): Methodological manual: 2018 edition. Publications Office. https://data.europa.eu/doi/10.2785/020714
[13] Hariri, Nizar. 2023. "Unprotected. Survey Report on The Challenges of The Current Social
Protection System in Lebanon Amidst the Crisis". Centre for Social Sciences Research & Action, Beirut: Lebanon.
Younes, Miriam. 2023. " A Decrepit Social Security Pillar. Salvaging the National Social Security Fund in Lebanon Amidst the Crisis". Centre for Social Sciences Research & Action, Beirut: Lebanon.
Scala, Michele. 2022. “An Intersectional Perspective on Social (in)Security. Making the Case for Universal Social Protection in Lebanon.” Centre for Social Sciences Research & Action, Beirut: Lebanon.
Abdo, Nabil. 2019. “Social protection in Lebanon: From a System of Privileges to a System of Rights.” Beirut: Arab NGO Network for Development.
[14] ILO. 2021. “Vulnerability and Social Protection Gaps Assessment – Lebanon.” ILO Prospect, 10 and 14.
[15] This refusal stems from the fact that the NSSF and the public sector cooperatives follow reimbursement schedules in Lebanese pounds, which are disconnected from healthcare bills denominated in US dollars. In the midst of the crisis, hospitals require individuals affiliated with publicly mandated programs to make substantial deposits (usually thousands of USD) in order to be admitted in case of emergencies or to access treatment.
[16] Abdo, Nabil. 2019. “Social protection in Lebanon: From a System of Privileges to a System of Rights.” Beirut: Arab NGO Network for Development.
Scala, Michele. 2022. “An Intersectional Perspective on Social (in)Security. Making the Case for Universal Social Protection in Lebanon.” Centre for Social Sciences Research & Action, Beirut: Lebanon.
Yehya, Hossam. 2015. La protection sanitaire et sociale au Liban (1860-1963). Ph.D. dissertation in Law. Nice: University Sophia Antipolis.
Calabrese, Erminia Chiara. 2020. « Le Hezbollah face à la « guerre » contre le Covid-19 », Les Carnets de l’Ifpo. La recherche en train de se faire à l’Institut français du Proche-Orient, https://ifpo.hypotheses.org/10355.
[17] Cammett, Melani and Issar Sukriti. 2010. “Bricks and Mortar Clientelism: Sectarianism and the Logics of Welfare Allocation in Lebanon.” World Politics 62 (3): 381-421.
